What Are Esophageal Varices? Causes, Symptoms, and Treatment Explained
Did you know that nearly 10 million people in India suffer from liver cirrhosis, a leading cause of deadly complications like esophageal varices? These swollen veins in the esophagus are a silent threat, often showing no symptoms until they burst, causing life-threatening bleeding. With liver disease cases rising, early detection and treatment of esophageal varices have never been more critical. Studies show that 30% to 40% of cirrhosis patients develop esophageal varices, and without proper intervention, 50% of these cases may lead to severe bleeding. Timely diagnosis and treatment could make all the difference in preventing these life-threatening complications.
What Causes Esophageal Varices?
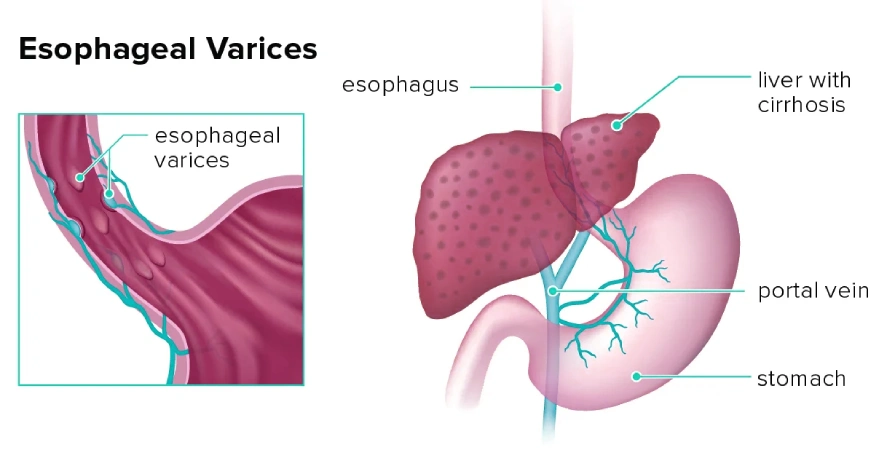
Esophageal varices are typically caused by portal hypertension, a condition where there’s increased pressure in the portal vein that carries blood to the liver. This pressure build-up is usually a result of liver damage, most commonly due to cirrhosis. As the liver becomes scarred and unable to function properly, blood flow is restricted, causing the blood to back up into smaller veins, like those in the esophagus, leading to varices.
Cirrhosis itself can be caused by chronic alcohol consumption, hepatitis B or C infections, or fatty liver disease. While liver disease is the primary cause of esophageal varices, other conditions, such as blood clots in the portal vein or parasitic infections like schistosomiasis, can also contribute to their development.
What Are the Symptoms of Esophageal Varices?
Esophageal varices may not show any symptoms unless they start to bleed, which is why regular monitoring is essential for people with liver disease. However, when they rupture and bleed, the symptoms can be alarming and may include:
- Vomiting blood: This is the most obvious and immediate symptom, often signaling a medical emergency.
- Black, tarry stools: This can occur due to the blood being digested in the gastrointestinal tract.
- Lightheadedness or fainting: This is caused by significant blood loss, which can lead to shock.
- Jaundice or abdominal swelling: These are signs of liver disease and portal hypertension, which may indicate the risk of varices.
If you experience any of these symptoms, seek medical attention immediately, as bleeding esophageal varices are a medical emergency.
How Are Esophageal Varices Diagnosed?
- Endoscopy: This is the most common diagnostic tool where a thin, flexible tube with a camera is inserted into the esophagus to visually check for varices.
- Imaging tests: CT scans, MRIs, or ultrasounds can be used to assess the liver, spleen, and blood flow in the portal vein.
- Blood tests: These can help evaluate liver function and detect any signs of portal hypertension, which can lead to varices.
Regular screening for esophageal varices is crucial for people with cirrhosis or other liver diseases to prevent life-threatening bleeding.
What Are the Treatment Options for Esophageal Varices?
- Medications:
- Beta-blockers help reduce pressure in the portal vein, lowering the risk of variceal bleeding, while vasoactive drugs are used to reduce blood flow and slow bleeding if it has already started.
- Endoscopic Treatment:
- Endoscopic variceal ligation (EVL): This is the most common treatment where a band is placed around the varices during an endoscopy to cut off the blood flow, causing the varices to shrink and eventually disappear.
- Endoscopic sclerotherapy: In this procedure, a solution is injected into the varices, causing them to collapse and harden. This method is used less often than EVL but can still be effective in stopping bleeding.
- Surgical and Radiological Procedures:
- Transjugular intrahepatic portosystemic shunt (TIPS): This procedure involves creating a new pathway for blood flow to bypass the liver, relieving the pressure in the portal vein and reducing the risk of bleeding. It’s often recommended for patients who haven’t responded well to other treatments.
- Liver transplant: In cases of advanced liver disease, a liver transplant may be necessary to address the underlying cause of the varices and prevent further complications.
- Managing Acute Bleeding:
- In cases of active bleeding, immediate measures such as balloon tamponade (temporarily stopping bleeding by applying pressure to the varices) or emergency endoscopic treatments are often required. Patients may also need blood transfusions to stabilize their condition.
What Can Be Done to Prevent Esophageal Varices?
Preventing the formation of esophageal varices involves managing the underlying liver condition. Some preventive strategies include:
- Managing cirrhosis: Following a liver-friendly diet, avoiding alcohol, and adhering to prescribed medications can slow the progression of liver disease and reduce the risk of varices.
- Regular screenings: If you have liver disease, regular check-ups with a gastroenterologist can help detect varices early and initiate preventive treatment before complications arise.
Esophageal varices, though a serious complication of liver disease, can be effectively managed with timely treatment and preventive care. Early detection and the right interventions are key to preventing life-threatening bleeding. If you or a loved one is dealing with liver disease or has been diagnosed with esophageal varices, consult an experienced specialist to explore your treatment options.
At Globus Gastroenterology Hospital, Dr Vedant H. Karvir, best Hepato Gastroenterologist in Mumbai, provides expert care for patients with liver disease and esophageal varices. With his extensive experience in managing complex gastrointestinal conditions, Dr. Karvir ensures personalized treatment plans that prioritize patient safety and well-being. Book your appointment today for a comprehensive consultation and expert guidance on managing esophageal varices.
Others Condition:
Bloating | Cancers of Stomach, Intestine & Liver | Constipation | Hirshsprung’s Disease | Gallstone | Dysphagia | Inflammatory Bowel Disease | Pancreatitis | SIBO | Barrett’s Esophagus | Blood in Stools / Vomitus | Celiac Disease | Diarrhea | Fatty Liver | Gerd | Irritable Bowel Syndrome | Piles



